corneal-cotton or saline drop will blink test|corneal reflex test syringe : manufacturer Though many are noninvasive in nature, they still involve alterations in blinking patterns or bright illumination, which can affect results. As such, it is recommended that any dry eye diagnostic test be performed in a .
Windows XP2 Build 2. Windows Longhorn Simulator (by mrfunnylaughs) Windows XP Simulator (by A Guy) .
{plog:ftitle_list}
At Villa Maria, our student life programs enthusiastically support every student’s interest. Choose from a vast array of activities to nurture a current interest or develop new ones. Participate in Villa's rich traditions, like Kairos, Senior Sing, or Carol and Ring. Showcase your talent by writing for a Villa publication. Try out for a sport .
The corneal reflex test (blink test) examines the reflex pathway involving cranial nerves V and VII. Classically the provider lightly touches a wisp of cotton on the patient’s cornea. This foreign body sensation should cause .
moisture meter for ceiling
In patients with normal corneal sensation, they typically reflexively blink, flinch, or even recoil when the testing tool is touched to their corneal surface. If the patient has abnormal sensation, they may report barely feeling . Brainstem reflex tests evaluate the function and integrity of the brain stem, a critical area controlling vital life functions such as consciousness, breathing, and heart rate. Assessment of the Corneal Reflex: The corneal reflex can be assessed through the following methods: Cotton wisp test: A soft cotton wisp or sterile gauze is gently touched .
A variety of techniques were employed for corneal reflex testing, the most common being "light cotton touch" (59.2%), followed by "cotton-tipped applicator with pressure" (23.9%), "saline or . Though many are noninvasive in nature, they still involve alterations in blinking patterns or bright illumination, which can affect results. As such, it is recommended that any dry eye diagnostic test be performed in a .The examiner will test for both afferent sensory and motor responses by observing whether the patient perceives the stimulus (sterile cotton swab or wisp of cotton) and concurrently blinks .
If the blink is normal, corneal sensation will be normal and there is no need for the test. If there is no blink, the eye is at risk. Look at the Figure and box below to see how the corneal sensation test is done.
Corneal fluorescein staining test: In all the experimental subjects, 90 sec after the TBUT, the corneal staining rate was assessed using the slitlamp biomicroscope with a cobalt blue filter; and .
Ocular motor cranial neuropathy (CN III, IV, VI) or skew deviation may be present in comatose patients. In CN III palsy the eye is typically down and out (hypotropia and exotropia) and CN VI palsy the eye is typically deviated inward (esotropia). A lesion involving the frontal eye fields results in conjugate deviation towards the side of the .
Hamano et al. modified Schirmer's test using a cotton thread impregnated with phenol red dye . the time from the last blink of the eye to the first dry spot on the tear film is measured under a cobalt blue filter. . for doctors to deliver 2 μL of 2% sodium fluorescein eye drops or fluorescein sodium strips soaked in physiological saline or . Instead, try to rinse your eye out. A saline solution (like contact solution) works best. To properly flush out your eye, use an eyecup or small, sanitized glass and hold it against the bone beneath your eye socket. With your upper eyelid held away from the cornea, tip the glass so that the saline solution washes out your eye. If you have a container of saline, eye wash or a gentle multi-purpose contact lens solution handy, feel free to use it, advises Dr. Bajic. Just avoid “super cleaning” solutions or solutions .
a. Jones I test: perform dye disappearance test, then attempt to recover fluorescein in inferior nasal meatus with cotton-tipped applicator after 5 minutes; abnormal result (no fluorescein) occurs in 33% of normal individuals. If the dye is retained in cotton-tipped applicator, the cause of tearing is probably hypersecretion i.e. epiphora. b. . The easiest ways to test corneal sensitivity include the use of a cotton wisp from a sterile swab, or from a strand of dental floss. Alternatively, there are more standardized ways to assess corneal sensitivity, such as via a handheld aesthesiometer, like the Cochet-Bonnet aesthesiometer, (however this is rarely available, or utilized in .
The Optrex ™ Dry Eye Blink Test is advertised as a rapid online test to indicate whether an individual might have dry eye. Like the clinical tear breakup test, it reflects the stability of the tears, however, in this test the time taken for the eyes to sense ocular discomfort is the measure for dry eye rather than the clinical assessment of . Blink characteristics may also play a role in dry eye symptoms. With the increase in digital device use, blink rates are reduced, which can exacerbate symptoms. One simple test to determine a reduced blink rate is to watch the patient use a digital device for 15 seconds, counting the number of blinks.Prescription eye drops may not be used over the contact lens. If feeling dry you may use Refresh Tears®, Refresh® Relieva, or Blink contacts® lubricating eye drops as needed. Lens care and solutions. Preservative Free Saline solutions. Examples include Addipak Sterile Saline Solution, Nutrifill, and LacriPure saline solution. The International Dry Eye Workshop Dry Eye Workshop (DEWS) defined dry eye as “a multifactorial disease of the tears and ocular surface that results in symptoms of discomfort, visual disturbance and tear film instability with potential damage of the ocular surface. It is accompanied by increased osmolarity of the tear film and inflammation of the ocular surface”.1 .
The human eye, a vital organ for vision, is a complex and sensitive structure that can be affected by various conditions, one of which is the production of excessive tears, medically known as epiphora or watery eyes. This condition, where tears overflow onto the face, can be due to either an overproduction of tears or inadequate drainage. Watery eyes are a common .
A drop of 2% fluorescein is placed at the lateral canthus, and the patient is asked to blink. With the lids open, there should be a 1-mm tear film along the upper and the lower eyelid margin. A poor tear film may indicate dry eye syndrome (keratitis sicca). Corneal staining may also be examined at this point. Tear Break-up Time
testing for corneal sensitivity
3. Dr Laurie Sullivan 2011Dr Laurie Sullivan 2011 Useful ToolsUseful Tools Slit lamp / magnificationSlit lamp / magnification Fluorescein stain [either strips orFluorescein stain [either strips or drops (2%)]. Stains corneal stroma,drops (2%)]. Stains corneal stroma, i.e. epithelial defect.i.e. epithelial defect. Local anaesthetic dropsLocal anaesthetic drops cotton buds, fine .Multiple vertically orientated linear abrasions should raise suspicion of a tarsal plate foreign body. The Seidel’s test using 2% fluorescein can detect an aqueous leak that will occur in non–self sealing corneal perforations. Differential diagnosis. A corneal abrasion with no foreign body is a possible alternative diagnosis.For me these felt more natural than saline or any other drop. Before inserting my lenses, I also would put two drops of Tears Naturelle in each lens and roll it around so it covers the entire inside of the lens before filling with saline.this provided a more comfortable cushioned feeling than saline alone. . because the lens still needs to .
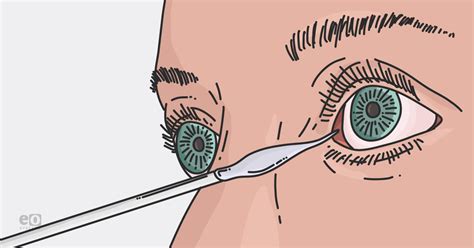
Wisp of cotton 3. Sterile drop of saline 4. Tip of a 1 mL syringe3. Sterile drop of saline Rationale: The client who is unconscious is at risk of corneal abrasion. The safest way to test the corneal reflex is by using a drop of sterile saline. Options . Medications: Dry eye is a side effect of medications for certain conditions, such as: high blood pressure; depression; colds and allergies; Laser eye surgery: Some types of laser surgery may .The corneal reflex, also known as the blink reflex or eyelid reflex, [1] is an involuntary blinking of the eyelids elicited by stimulation of the cornea (such as by touching or by a foreign body), though it could result from any peripheral stimulus. Stimulation should elicit both a direct and consensual response (response of the opposite eye). The reflex occurs at a rapid rate of 0.1 seconds.The management of corneal abrasions has largely excluded dispensing topical local anesthetics for home use due to concern for corneal toxicity. We have reviewed and critically appraised the available literature evidence regarding the use of topical anesthetics in patients with simple corneal abrasions. Using sequential Delphi review, we have developed these clinical .
White blood cells may also enter several layers of the cornea, which can increase corneal edema and put these tissues at risk of further damage. Toxicity: Chemicals entering the eye, whether due to eye surgery or from an accident, can cause damage to the cornea that leads to swelling. Toxic effects may be acute and require hospital treatment .
Additionally, you should also avoid any eye drops without asking your doctor first. Keep in mind that there are no over-the-counter eye drops that can treat eye scratches. Once you schedule an appointment with your eye care service provider, they will treat your corneal abrasion with antibiotic eye drops or ointment.It can also be used to detect foreign bodies on the surface of the eye, and determine if there is an injury to the eye or eye infection. The test is performed by administering dye onto the eye's surface. After the dye has thoroughly covered the eye a cobalt blue light is then directed on the eye. The light causes the dye to glow green.
A healthcare professional may perform a diagnostic test using a dye to determine if you have a corneal abrasion. The dye will illuminate the scratched area. Corneal Abrasion vs. Ulcer. A corneal abrasion is not the same as a corneal ulcer. However, a corneal abrasion may result in a corneal ulcer. A corneal ulcer refers to an open sore on the .Study with Quizlet and memorize flashcards containing terms like A client sustains an injury to the brain stem. What is the most important assessment parameter that the nurse should perform for this client? Depth of respirations Movement of all extremities Level of consciousness Sensation in extremities, A nurse is testing a client's corneal reflex but notices that the reflex appears to be .
Corneal reflex testing remains a cornerstone of the coma exam and is commonly used in neuroprognostication of unconscious cardiac arrest survivors and in brain death determination. . the most common being "light cotton touch" (59.2%), followed by "cotton-tipped applicator with pressure" (23.9%), "saline or water squirt" (15.9%), and "puff of . The panel strongly recommended a test of corneal sensitivity in patients with a painless epithelial defect, or a persistent epithelial defect that does not improve within 14 days [].The panel also strongly recommended such a test in patients with a history of herpetic eye disease and in patients who have had procedures that might have damaged the trigeminal .
sterile corneal reflex test
Resultado da We would like to show you a description here but the site won’t allow us.
corneal-cotton or saline drop will blink test|corneal reflex test syringe